Athlete’s Foot (Tinea Pedis)
Athlete’s foot is a contagious fungal infection that causes different itchy skin issues on your feet. An itchy, stinging, burning rash forms on infected skin. Athlete’s foot treatment can stop the fungus from spreading and clear it up.
Overview
What is athlete’s foot?
Athlete’s foot is a common fungal infection (caused by a fungus). Athlete’s foot causes an itchy, stinging, burning rash on the skin on one or both of your feet. Athlete’s foot is most common between your toes, but it can also affect the tops of your feet, the soles of your feet and your heels. Your skin may become scaly and cracked or develop blisters. Sometimes, your feet smell bad.
Athlete’s foot is a form of ringworm. “Tinea pedis” is another name for athlete’s foot. “Tinea” is another name for ringworm, and “pedis” means foot or feet.
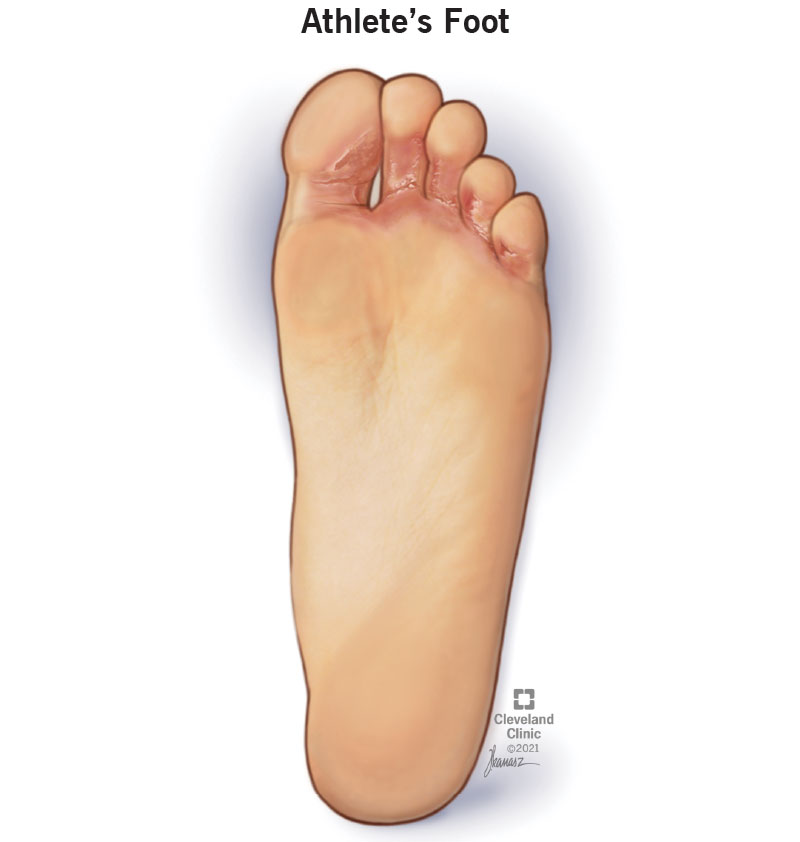
What does athlete’s foot look like?
Athlete’s foot can affect the skin between your toes, the bottoms of your feet, the tops of your feet, the edges of your feet and your heels. Your skin may appear irritated (red, purple, gray or white), scaly or flaky.
Who is at risk?
Athlete’s foot affects everyone. However, it most commonly affects men (and people assigned male at birth) and people over the age of 60. You may be more likely to develop athlete’s foot if you have:
How common is athlete’s foot?
Athlete’s foot is common. Estimates suggest that 3% to 15% of the population has athlete’s foot, and 70% of the population will have athlete’s point at some time in their lives.
Symptoms and Causes
What are the symptoms of athlete’s foot?
Symptoms of athlete’s foot include:
- Cracked and peeling skin.
- Itchy skin.
- A skin rash.
- A burning sensation.
What are the different types of athlete’s foot?
Your symptoms depend on the type of athlete’s foot that you have.
- Toe web infection: A toe web infection is the most common type of athlete’s foot. It typically affects the skin between your fourth toe (ring toe) and fifth toe (pinkie toe). Your skin may change color, crack, peel or flake.
- Moccasin-type infection: A moccasin-type infection affects the bottoms of your feet, your heels and the edges of your feet. Your feet may be sore for a few days. Then, the skin on the bottoms of your feet thickens and cracks. In rare cases, your toenails may get infected. They can thicken, break into small pieces and fall out.
- Vesicular-type infection: A vesicular-type infection typically affects the bottoms of your feet, but it may appear anywhere on your feet. A vesicular-type infection features bumps or fluid-filled blisters (vesicles).
- Ulcerative infection: An ulcerative infection is the rarest type of athlete’s foot. Open sores (ulcers) often appear between the toes. Open sores may also appear on the bottoms of your feet.
What causes athlete’s foot?
Several different species of fungi cause athlete’s foot.
It commonly spreads through skin-to-skin contact or contact with a flake of skin. It spreads in areas used by large groups of people, like locker rooms, swimming pools and saunas.
It can also spread through contact with an infected surface. You can get athlete’s foot by sharing towels, socks or shoes with someone who has athlete’s foot.
Is athlete’s foot contagious?
Athlete’s foot is contagious. It’s a fungus that grows on or in your skin. Fungi (plural form of fungus) need warm temperatures and moisture to grow. People often wear socks and tight shoes every day, which keep their feet warm and moist. This is the perfect environment for athlete’s foot to grow.
Diagnosis and Tests
How is athlete’s foot diagnosed?
Your healthcare provider can typically diagnose athlete’s foot by examining your feet and symptoms.
What tests will be done to diagnose athlete’s foot?
In some cases, your healthcare provider may remove a small piece of skin (biopsy) and test it in a lab. Several drops of a potassium hydroxide (KOH) solution dissolve the skin cells so only fungal cells are visible.
Management and Treatment
How do I treat athlete’s foot?
Over-the-counter (OTC) and prescription antifungal creams, ointments, gels, sprays or powders effectively treat athlete’s foot. These products contain clotrimazole, miconazole, tolnaftate or terbinafine.
Some prescription antifungal medications for athlete’s foot are pills. These pills contain fluconazole, itraconazole or terbinafine.
It’s important to finish your full course of medicine. If you stop too soon, your athlete’s foot may come back and be harder to treat.
How do I manage my athlete’s foot symptoms?
Keep your feet dry, clean and cool. If possible, don’t wear socks or shoes. Avoid scratching your feet. Scratching your feet may cause the fungus to spread to other parts of your body.
How soon after treatment will I feel better?
With proper diagnosis and treatment, your athlete’s foot should go away in one to eight weeks. Follow your healthcare provider’s instructions.
It’s important to finish your full course of medicine. During the early healing stages, itchiness and irritation will fade. Even if your symptoms go away, you may still have athlete’s foot. If you don’t finish your full course of medicine, your athlete’s foot can come back and be harder to treat.
What will happen if athlete’s foot is left untreated?
Athlete’s foot can spread across the bottom of your foot. This is moccasin athlete’s foot. In feet with moccasin athlete’s foot, the skin on the bottoms, heels and edges of your feet are dry, itchy and scaly.
In severe cases of athlete’s foot, you may develop fluid-filled blisters or open sores. Blisters often appear on the bottoms of your feet, but they may develop anywhere on your feet. Open sores often appear between your toes, but they may appear on the bottoms of your feet. Your feet may also smell bad.
Athlete’s foot doesn’t typically go away on its own. If it’s left untreated, it can spread to other areas of your body, including your:
- Nails: Fungal nail infections can be more difficult to treat. They’re often more resistant to many treatments.
- Hands: A similar fungal infection can spread to your hands. This happens when you scratch your infected feet or use the same towel to dry off your infected feet and hands.
- Groin: The same fungus that causes athlete’s foot can also spread to your groin. It’s a condition called jock itch. The fungus typically spreads from your feet to your groin after using a towel to dry off after bathing or swimming.
Prevention
How can I reduce my risk of athlete’s foot?
There are many ways to reduce your risk of getting athlete’s foot:
- Thoroughly wash your feet and the skin between your toes with antibacterial soap.
- Dry your feet and the spaces between your toes after swimming or bathing.
- Apply talcum powder or antifungal powder to your feet to absorb moisture.
- Put on your socks before your underwear to prevent the fungus from spreading to your groin.
- Wear shoes or sandals that allow your feet to get air.
- Avoid wearing rubber or synthetic shoes for long periods.
- Allow your shoes to dry out for at least 24 hours between uses.
- Clean your shoes with disinfecting sprays or wipes.
- Wear cotton or wool socks that absorb moisture or socks made out of synthetic materials that wick away moisture.
- Wear sandals or flip-flops in communal locker rooms, pools, saunas or showers.
- Wash your socks, towels and bedding in hot water.
Outlook / Prognosis
What can I expect if I have athlete’s foot?
With proper treatment, the outlook for people with athlete’s foot is good. Be sure to follow your healthcare provider’s instructions so you get rid of your athlete’s foot quickly and don’t pass it on to anyone else.
Living With
When should I see my healthcare provider?
Call your healthcare provider if your athlete’s foot:
- Doesn’t improve or go away with treatment.
- Looks infected (red, purple, gray or white skin; irritation and swelling).
- Spreads to other areas of your body.
What questions should I ask my doctor?
- How did I get athlete’s foot?
- How long is athlete’s foot contagious?
- Should I avoid going to the gym, public pool, sauna or other public places?
- What steps can I take to prevent athlete’s foot from spreading to other parts of my body?
- What steps can I take to prevent athlete’s foot from spreading to other people?
- What’s the best treatment for athlete’s foot?
- Should I avoid any medications or treatments?
- What steps can I take to keep from getting athlete’s foot again?
- Should I look out for signs of complications?
A note from Cleveland Clinic
Athlete’s foot is an unpleasant condition. It’s itchy and annoying. It can also sting or burn and smell bad. However, antifungal medications or home remedies will help you get rid of athlete’s foot. Remember, you shouldn’t scratch your athlete’s foot, as it can spread to other parts of your body. It’s important to follow your healthcare provider’s treatment plan. If you don’t finish your full course of medicine, athlete’s foot can come back. Ask your healthcare provider how you can keep athlete’s foot from spreading to other parts of your body or other people.


